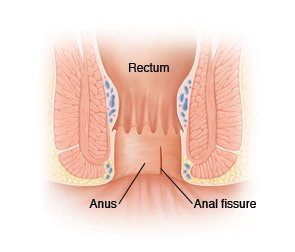
 An anal fissure (fissure-in-ano) is a small, oval shaped tear in skin that lines the opening of the anus. Fissures typically cause severe pain and bleeding with bowel movements. Fissures are quite common in the general population, but are often confused with other causes of pain and bleeding, such as hemorrhoids.
An anal fissure (fissure-in-ano) is a small, oval shaped tear in skin that lines the opening of the anus. Fissures typically cause severe pain and bleeding with bowel movements. Fissures are quite common in the general population, but are often confused with other causes of pain and bleeding, such as hemorrhoids.
Symptoms of an Anal Fissures
The typical symptoms of an anal fissure include severe pain during, and especially after, a bowel movement, lasting from several minutes to a few hours. Patients may also notice bright red blood from the anus that can be seen on the toilet paper or on the stool. Between bowel movements, patients with anal fissures are often relatively symptom-free. Many patients are fearful of having a bowel movement and may try to avoid defecation secondary to the pain.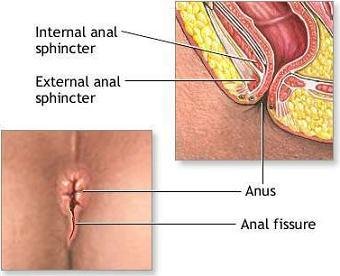
Pathophysiology of Anal Fissures
Fissures are usually caused by trauma to the inner lining of the anus. Patients with tight anal sphincter muscles (i.e., increased muscle tone) are more prone to developing anal fissures. A hard, dry bowel movement is typically responsible, but loose stools and diarrhea can also be the cause. Following a bowel movement, severe anal pain can produce spasm of the anal sphincter muscle, resulting in a decrease in blood flow to the site of the injury, thus impairing healing of the wound. The next bowel movement results in more pain, anal spasm, decreased blood flow to the area, and the cycle continues. Treatments are aimed at interrupting this cycle by relaxing the anal sphincter muscle to promote healing of the fissure.
Treatment of Anal Fissures
The majority of anal fissures do not require surgery. The most common treatment for an acute anal fissure consists of making the stool more formed and bulky with a diet high in fiber and utilization of over-the-counter fiber supplementation (totaling 25-35 grams of fiber/day). Stool softeners and increasing water intake may be necessary to promote soft bowel movements and aid in the healing process. Topical anesthetics for pain and warm tub baths (sitz baths) for 10-20 minutes several times a day (especially after bowel movements) are soothing and promote relaxation of the anal muscles, which may help the healing process.Other medications (such as nitroglycerin, nifedipine, or diltiazem) may be prescribed that allow relaxation of the anal sphincter muscles. Your surgeon will go over benefits and side-effects of each of these with you. Narcotic pain medications are not recommended for anal fissures, as they promote constipation. Chronic fissures are generally more difficult to treat, and your surgeon may advise surgical treatment.Fissures can recur easily, and it is quite common for a fully healed fissure to recur after a hard bowel movement or other trauma. Even when the pain and bleeding have subsided, it is very important to continue good bowel habits and a diet high in fiber as a lifestyle change. If the problem returns without an obvious cause, further assessment is warranted.A fissure that fails to respond to conservative measures should be re-examined. Persistent hard or loose bowel movements, scarring, or spasm of the internal anal muscle all contribute to delayed healing. Other medical problems such as inflammatory bowel disease (Crohn’s disease), infections, or anal tumors can cause symptoms similar to anal fissures. Patients suffering from persistent anal pain should be examined to exclude these symptoms. This may include a colonoscopy or an exam in the operating room under anesthesia.
Surgery for Anal Fissures
Surgical treatment for anal fissures involves surgical division of a portion of the internal anal sphincter (lateral internal sphincterotomy). The goal of surgery is to promote relaxation of the anal sphincter, thereby decreasing anal pain and spasm, allowing the fissure to heal. All surgical procedures carry some risk, and a sphincterotomy can rarely interfere with one’s ability to control gas and stool. Drs. Park and Itriago will discuss these risks with you to determine the appropriate treatment.It is important to note that complete healing with both medical and surgical treatments can take up to approximately 6-10 weeks. However, acute pain after surgery often disappears after a few days. Most patients will be able to return to work and resume daily activities in a few short days after the surgery.
